Deirdre Marzano MSW, LCSW, a HopeHealth Visiting Nurse social worker, met with Sarah,* who was making a speedy recovery after being discharged from the hospital on a mid-winter day.
Fifteen minutes into their 45-minute visit together, Deirdre asked Sarah if she had chosen a power of attorney for health care. If so, whom did she pick?
“I assume that my oldest daughter would be making these decisions,” Sarah told Deirdre.
March is National Social Work Month
The National Association of Social Workers has designated March the time to honor the contributions social workers like Deirdre make to the overall well-being of the communities they serve. Deirdre, who joined HopeHealth in October 2020, spent 18 years as a resident services coordinator for a public housing authority before going back to school to earn a master’s degree in social work. Her background has given her a deep understanding of the unique needs of seniors as they age.
Deirdre’s job is to find out what her patients need to safely recover in the comfort of their home. She makes referrals for meal deliveries and home care aide services or connects them to community resources to address other basic needs, financial or legal concerns. She might also help enroll income eligible patients in the state co-pay program that covers a portion of the cost of personal care and adult day services. Deirdre also acts as an advocate for her patients and might help them form ideas and questions to ask at their next doctor’s appointment.

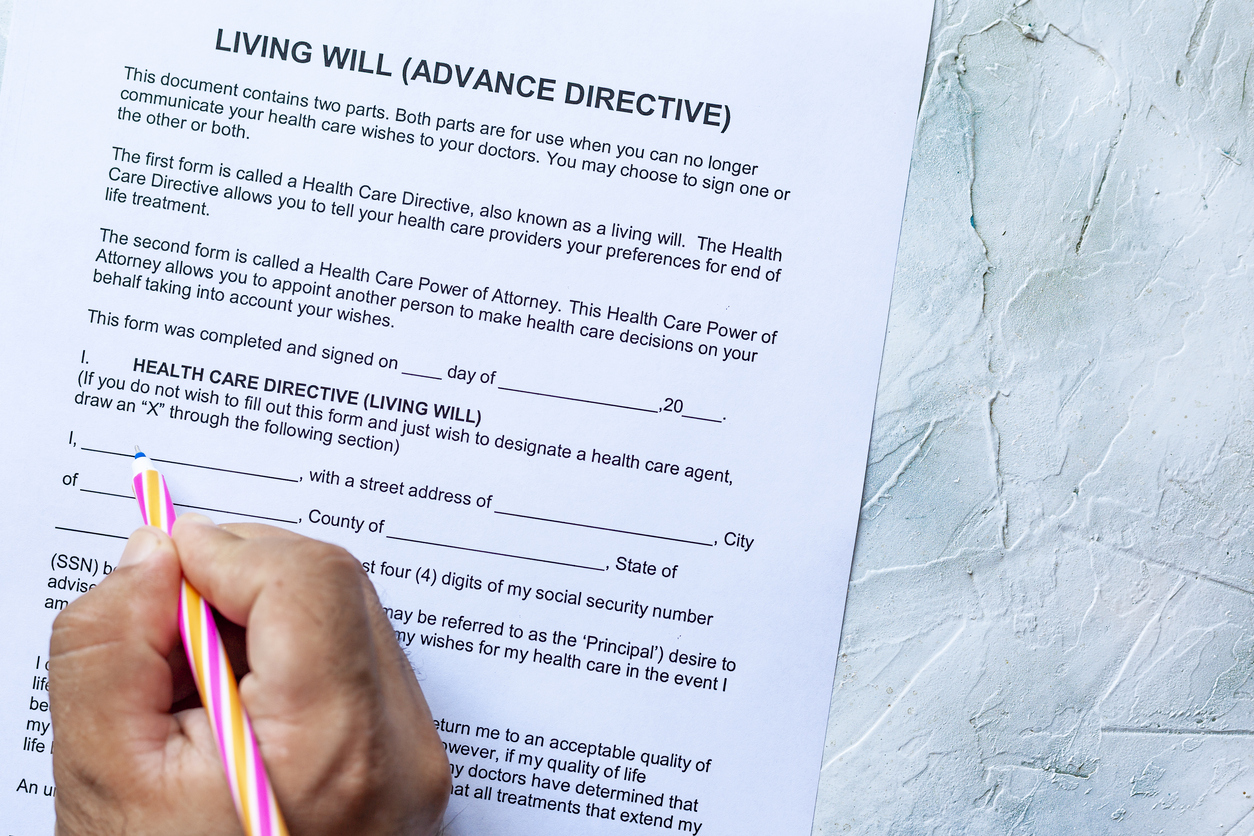
One of Deirdre’s essential roles as a social worker is to help patients understand and complete advance directives. These are the written instructions expressing what a person wants for their medical treatment if they are unable to communicate. While advance care planning is often thought of as a topic for old or sick people, it’s important for healthy people of all ages to take the time to think about what they would want to happen if they became incapacitated in the future.
An ideal time to introduce this topic is actually when a patient is feeling well, says Maria Appenfeller, RN, CHPN, manager of HopeHealth Visiting Nurse’s palliative program. Deirdre is one of two social workers assigned to the team Maria manages.
Thoughtful decision making is more likely when a person is not in pain or emotionally distressed, Maria says.
“Home is where you’re most comfortable,” Maria says. “Home is where we can see what your life is like rather than in the doctor’s office or in the emergency room or in a hospital bed.”

End-of-life planning means choosing how to live
End-of-life planning is not the easiest conversation to have during a pandemic when masks hide the smiles that help soften serious subject matter. But the pandemic also presents the opportunity to ask patients about their goals.
Sometimes, all Deirdre can do is introduce the topic of advance directives. It helps that she does so in a patient’s home where they are more likely to be relaxed and comfortable and even when the patient is actually feeling quite well and anticipating many good days still ahead. But Deirdre believes the earlier the subject comes up, the better prepared patients and their families will ultimately be for making decisions in the future.
“There are some people who just aren’t ready,” Deirdre says. “And that’s okay. You plant that seed.”

There’s a form for that
When it comes to making final wishes known, it’s best to ensure you have it in writing. Adult children might not know what their older parents want at end of life. That’s why Deirdre arrives for her home visits carrying a black tote bag full of pamphlets and forms. She calls it her “bag of goodies.”
Goodies like the Medical Orders for Life-Sustaining Treatment (MOLST), a pink form for patients with advanced illness to fill out indicating their wishes. The form lets patients check off their preferences for resuscitation and use of a ventilator or feeding tube. The MOLST should be placed on their refrigerator so it’s readily available in case any first responders are called to the home.
Another form is the Durable Power of Attorney for Health Care, which lets a patient appoint someone to make health care decisions for them when they cannot actively participate in decision making.
Both of these forms are available online, including through state department of health websites. But Sarah had not seen them before and wasn’t ready yet to start thinking about the forms when Deirdre brought them up.
“Oh, I really don’t want to talk about dying,” Sarah told Deirdre.
“I understand,” Deirdre replied. “May I offer this as a perspective? It’s allowing your loved ones to know how you choose to live.”
Deirdre also understands that patients fill out forms at their own pace. Sarah wanted to talk about her plans for the future, including finishing the autobiography she was writing.
Tools for another day
Medicare covers home visits for medical social services when ordered by a doctor to help a patient address social and emotional concerns. These are typically addressed during one to three visits over 30 days or sometimes 60 days if the patient’s recovery will take longer.
Sarah recovered and was back to living independently and writing her book in her home. She didn’t require a follow-up visit from Deirdre after their first meeting.
Deirdre thinks back on the impact starting the conversation about advanced directives may have made.
“She has the tools and that’s what’s important,” Deirdre says.
“As social workers we meet our clients where they’re at. We provide them with the information that may make things easier for them to make a decision.”
Maybe Sarah has looked at the forms and thought more about her options. Deirdre doesn’t know. But she knows she has done her job. And she knows winter is fading into spring.
She’s planted a seed.
*Patient names were changed to protect privacy.

