The surprising truth: Some patients live longer on hospice care
Published July 13, 2021
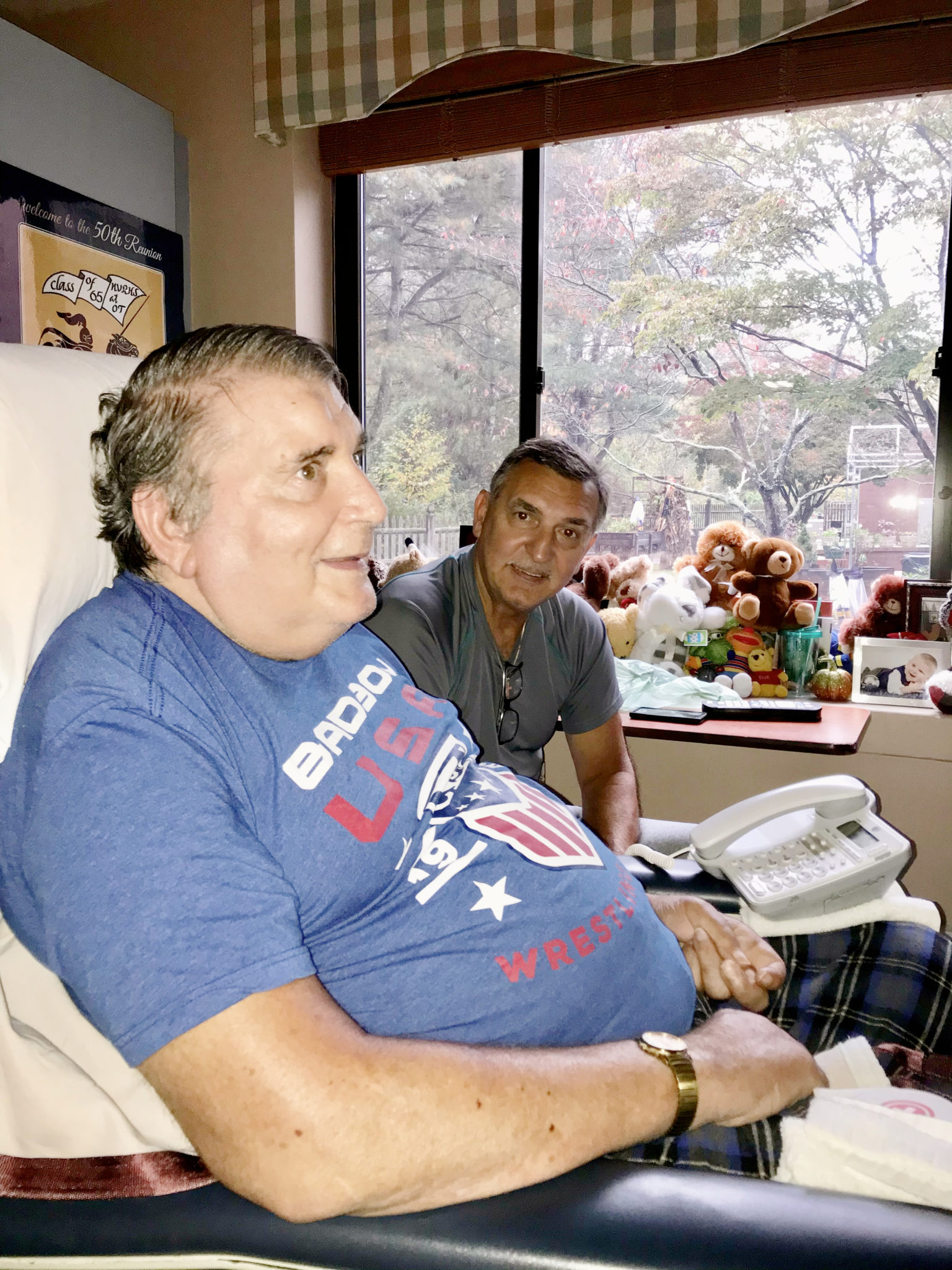
In October 2019, Serge DeLaulo, Jr., of Westerly, RI, passed away at age 72 after a valiant, lifelong battle with multiple sclerosis (MS). His family remembered him as a passionate Cribbage player and Yankees fan who loved spending time with members of his extended family and friends as well as children and grandchildren.
Carole Sobiechowski, Serge’s sister, takes comfort knowing her brother died the way he lived, on his own terms and with dignity, thanks to hospice care. Initially diagnosed with weeks to live, Serge rallied on hospice and lived another five months.
“I know he wouldn’t have lasted as long as he did without hospice. I think it gave him the summer,” Carole recalls.

How hospice can extend life expectancy
Serge’s unexpectedly long run on hospice is not a rare occurrence, according to several landmark studies on life expectancy among hospice and palliative care patients.
A 2007 report by the National Hospice and Palliative Care Organization (NHPCO) found that patients with certain terminal diseases who chose hospice lived an average of 29 days longer than similar patients who did not receive hospice. The findings not only dispel the myth that hospice hastens death but also suggest hospice could prolong life for patients with certain conditions.
How can someone with a terminal illness live longer on hospice? According to the NHPCO researchers, hospice patients are more likely to:
- Avoid the risks of over-treatment
- Receive additional monitoring and treatments only available through hospice
- Increase their desire to continue living due to the constant attention to their emotional wellbeing and physical health
“The goal of hospice is quality of life,” explains Edward Martin, MD, MPH, FAAHPM, Chief Medical Officer for HopeHealth. “We make sure every day is as good as possible and help patients get the best care possible in the home setting if that is, in fact, what they want to do.”
“We have a notion in this country that the more care you get, the better you're going to do,” Dr. Martin says. “But if we give chemotherapy to certain cancer patients who are quite ill, it may be a net harm for them.” —Dr. Edward Martin, HopeHealth
How patient-directed hospice care can reduce over-treatment
Hospice and palliative care providers evaluate all therapies and medications through the lens of quality of life. They also ask patients what they wish to accomplish, which is called a goals-of-care conversation.
For example, a patient might wish to celebrate an upcoming anniversary or birthday. If aggressive treatment will make them too sick to participate, the care team can present the pros and cons and let the patient decide.
For people with certain late-stage cancers, treatments like chemotherapy can have little benefit and even be harmful, says Dr. Martin.
“We have a notion in this country that the more care you get, the better you're going to do,” Dr. Martin says. “But if we give chemotherapy to certain cancer patients who are quite ill, it may be a net harm for them. We send them for procedures and tests and interventions—that’s the group least likely to have a benefit and most likely to have a complication.”
Hospice care providers also take a close look at patients’ medications taken for long-term maintenance of conditions like cholesterol or diabetes. Some of these prescriptions can cause loss of appetite or other side effects, which can interfere with quality of life or will to live.

Increased hospice monitoring leads to fewer hospitalizations
While on hospice Serge stayed at his nursing home under the watchful eye of Lisa Masucci, RN, case manager, and a HopeHealth hospice team. Lisa talked to Carole once or twice per week about Serge’s condition, medications and spirits.
“She was extremely thorough. She was amazing,” Carole recalls. “I never felt more in control of my brother’s care than when he was in hospice.”
“It’s the attention to detail—your nurse comes out regularly, noticing things, staying on top of symptoms,” Dr. Martin explains. “That close monitoring can pick up things early while you can still manage them at home,” resulting in fewer trips to the to the emergency department.
Can hospice patients live longer if they feel better?
Carole believes one reason Serge survived the summer is that hospice gave him more time with his family. “The people that knew and loved him got to be with him longer and he was grateful for that,” she adds.
Dr. Martin says some patients lose the will to live because they think they are burdening their families. Hospice care lifts that burden by surrounding patients with an array of medical and psychosocial supports that can brighten patients’ spirits and help the entire family.
Looking back on Serge’s experience, Carole says her view of hospice changed. “I’d always thought hospice was an ending, but this opened my eyes,” she says. “The whole disease he did it his way. He was in control of certain things, and they let him be in control. Hospice allowed him his dignity.”
“HopeHealth is an incredible organization. I'm certainly very grateful,” she adds.
Go deeper: What does science say about hospice and life expectancy?
Dr. Martin offered insight on three significant studies of hospice and palliative care.
Study #1 (2007): On hospice patients with congestive heart failure and certain cancers1
Findings: Hospice enrollment was not significantly associated with shorter survival and in some instances was associated with longer survival.
Significance: “For certain well-defined terminally ill populations, patients who choose hospice care live an average of 29 days longer than similar patients who do not choose hospice,” according to the study by hospice and palliative care providers.
Study #2 (2010): On hospice patients with advanced lung cancer2
Findings: A New England Journal of Medicine report found that early palliative care was associated with longer survival, less aggressive end-of-life care and improved quality of life and mood.
Significance: Dr. Martin calls the report “groundbreaking” in the field of hospice and palliative medicine because it led oncologists to embrace palliative care in their cancer centers.
Study #3 (2018): On hospice patients with advanced heart failure3
Findings: The Journal of the American College of Cardiology reported that patients on hospice used less health care, lived longer and were less likely to die in the hospital.
Significance: This study was notable because the researchers were cardiologists, not palliative care physicians, says Dr. Martin.
1. Connor SR, Pyenson B, Fitch K, Spence C, Iwasaki K. Comparing hospice and nonhospice patient survival among patients who die within a three-year window. J Pain Symptom Manage. 2007 Mar;33(3):238-46.
2. Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, Dahlin CM, Blinderman CD, Jacobsen J, Pirl WF. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2010;363(8):733–42.
3. Gelfman LP, Barrón Y, Moore S, Murtaugh CM, Lala A, Aldridge MD, Goldstein NE. Predictors of Hospice Enrollment for Patients With Advanced Heart Failure and Effects on Health Care Use. JACC Heart Fail. 2018 Sep;6(9):780-789.
Questions about eligibility for hospice or palliative care? Contact us at (844) 671-4673 or Information@HopeHealthCo.org.

