If you think sadness clouds the daily life of a hospice and palliative doctor, think again.
“Truth be told, caring for people with serious illness can bring joy,” says Christine Nevins-Herbert, MD, who practices at HopeHealth Hulitar Hospice Center while also seeing HopeHealth patients at Miriam Hospital in Providence, RI.
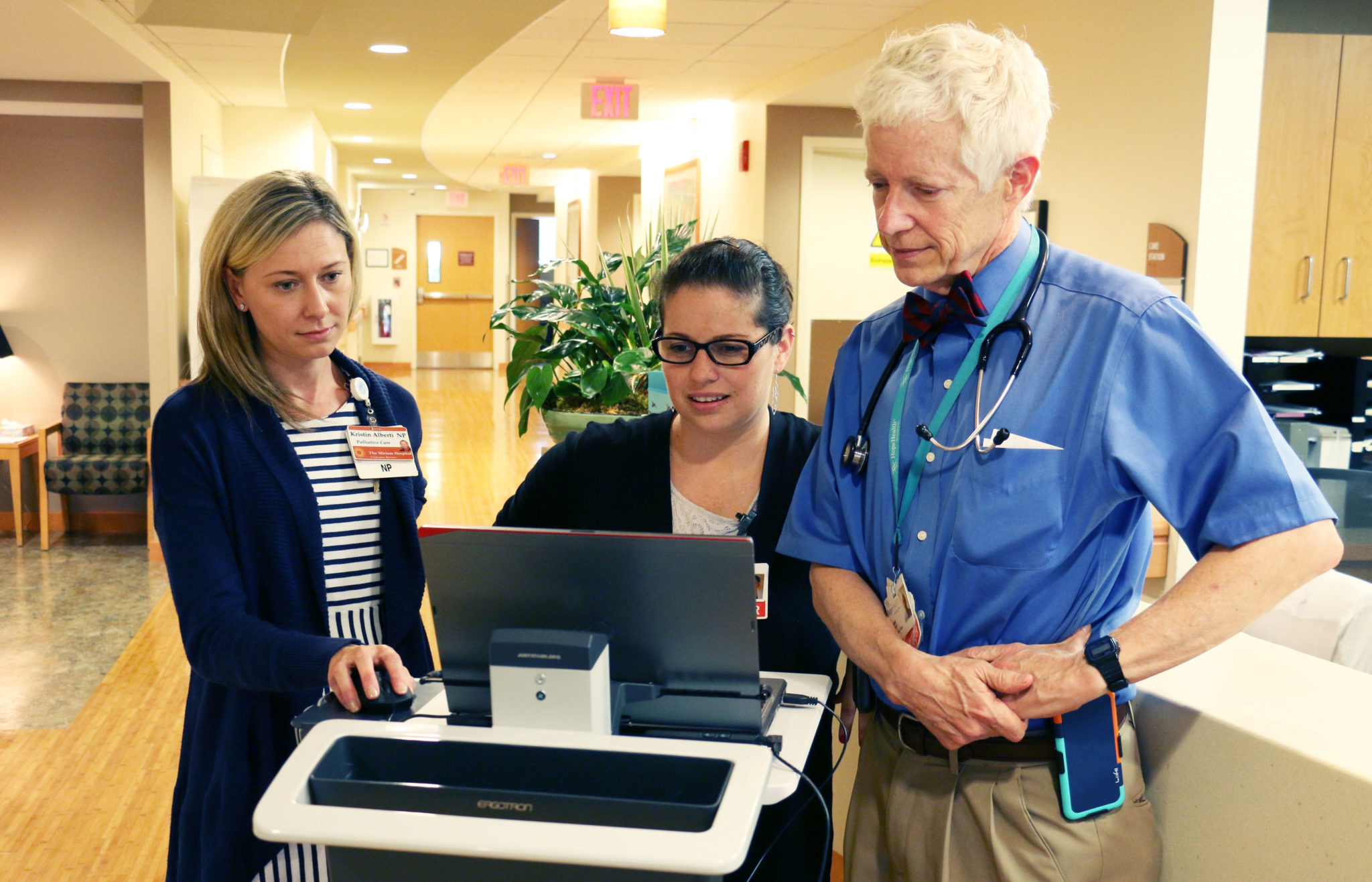
Dr. Nevins-Herbert is one of HopeHealth’s several board-certified hospice and palliative care physicians. The team provides care in hospitals, nursing homes, assisted living facilities and patients’ homes throughout Rhode Island and Massachusetts.
Bilingual in Spanish, Dr. Nevins-Herbert is a clinical professor at Brown University’s Warren Alpert School of Medicine and an expert in communicating the issues of complex care. In this Q&A, she discusses what makes her job special.
“It’s an honor to be with people in their darkest and most difficult times, and be able to help them find some hope or silver lining.”
HopeHealth: Why did you decide to specialize in hospice and palliative care?
I always had a pretty severe fear of death and dying when I was growing up. I knew that fear would be tough to overcome, so when in medical school, I somewhat reluctantly decided to do an elective in hospice and palliative care.
I quickly realized that end-of-life care isn’t all about dying and sadness. It’s actually about life and hope.
It’s our job to ensure that even when people are nearing the end of their lives that we are doing what is in their best interest. We are asking them what matters and making sure people still have a voice and the opportunity to live the best they can.
I ended up choosing to do a family medicine residency. Throughout my residency, there was a common thread: all of the most rewarding, impactful and energizing cases were around end of life or helping someone through the tough time of hearing a serious diagnosis. Soon, the topic I originally was too afraid to think of ended up becoming my passion and life’s work.
It’s an honor to be with people in their darkest and most difficult times, and help them reframe the situation to find some hope, a silver lining or try to lessen their pain.

What kinds of issues are your patients are dealing with?
Really, it can be anything—heart disease, lung disease, kidney disease, liver disease, cancer, Alzheimer’s—any advanced illness.
We can see patients in the emergency room or after they have been in the hospital for days or sometimes weeks. Ideally we want to see them earlier in their hospitalization.
What is the difference between palliative care and hospice care?
Palliative care is about improving quality of life for patients with any stage of a serious or chronic illness. Palliative care is a much bigger umbrella, it’s not just for people at the end of their life. All hospice care is palliative, but not all palliative care is hospice. (Learn more about the differences between hospice and palliative care here.)
What does it mean to be board-certified in hospice and palliative medicine?
It means we are experts in our field. To be certified, you must do a fellowship in hospice and palliative medicine, then pass the board exam in that specialty. We really take pride in that additional training and have committed our careers to this.
“There is always more we can do to help you feel comfortable or loved or supported or safe. There is always something to be hopeful for.”
What about your job is special?
Some of the most powerful and rewarding cases are where you start the encounter or relationship, and the patient and family are nowhere near ready to accept the reality of how sick a loved one is.
By the end of the encounter or after one or two hospitalizations, you sort of have planted enough seeds and introduced palliative care in a way that has optimized their understanding, so the concept has had enough time to grow and flourish.
Sometimes that ah-ha moment is really powerful. A patient or family member says, “Oh, I see what you have been talking about. Maybe coming back and forth to the hospital every couple of weeks isn’t the best way for my loved one to live the rest of their life.” Then we can think about things in a different way. Perhaps that is when we make the choice to shift from curative care to comfort care.
Those are some of the most powerful cases, where something changes over time and there is that realization and acceptance.

What you’re describing is denial and a fear of death, right?
Sure. A lot of people describe their loved ones as fighters: “He is a fighter and he is going to come through this.”
I respond by saying, “Absolutely he is a fighter, or he wouldn’t have made it this far. But what does it make sense to be fighting for now?” That may be something different than it was a few months ago or a few years ago.
So how do you help the individual and family work through that?
One of my favorite parts of my job is helping people reframe hope. Rather than taking hope away or saying, “Forget about that, it’s not going to happen,” we share in whatever their hope is: hope for a cure, hope for a miracle, hope they will get better.
When doctors or people say there is nothing more we can do, that is never true. There is always more we can do. It may not be, “What more we can do to cure your terminal illness?” but there is always more we can do to help you feel comfortable or loved or supported or safe. There is always something to be hopeful for.